Day 1 :
Keynote Forum
Cliodhna Foley-Nolan
Director of Human Health & Nutrition, Safefood, Ireland
Keynote: Cost of a Healthy Food Basket

Biography:
Dr Foley-Nolan MB,BCh,BAO,DCH,DObs,MPH,FFPHM is Director of Human Health and Nutrition with safefood, the all –island Food Safety Promotion Board. She directs the public health and nutrition functions of the organisation. Cliodhna has a medical degree from UCC; a master’s in Public Health from UCD and is a fellow of the Faculty of Public Health of the Royal College of Physicians in Ireland. She has worked at consultant level in Public Health Medicine in the Health Services Executive, and is a specialist in the areas of health promotion and foodborne infectious disease.
Dr Foley-Nolan holds a Senior lecturer post in UCC and is a trainer and examiner at the Royal College of Physicians in Ireland. She has served on many national advisory groups including those on the National Strategy for the Control of Antimicrobial Resistance, the National AIDS Advisory Group and the National Healthy Eating Guidelines group. She has served on the boards of the Food Safety Authority of Ireland and the Veterinary Council of Ireland. She is currently a board member of the Obesity Prevention Steering Group in Northern Ireland, the Special Advisory Group on Obesity in the Republic of Ireland, the Royal College of Physician’s obesity specialist group and the Health Research Board Centre for Diet and Health.
Abstract:
Statement of the Problem: Children of low income households eat less well and have higher rates of childhood obesity and associated risks (1,2). Childhood obesity tracks into adulthood. Food is often a flexible component of the family budget as they can satisfy their hunger with cheaper, less nutritious food (3). This research uses an approach that identifies and costs a basket that is both socially acceptable and nutritionally adequate. One in ten people are experiencing food poverty in Ireland (4). Methodology and Theoretical orientation: A Minimum Essential Standard (MIS) approach was used (5) to estimate the income needed to afford a weekly food basket that the six households studied agreed as a minimum (for urban and rural settings). The study also estimated the % spend on food relative to other items of expenditure. Findings: The cost of the food Basket was more expensive for the majority of rural households compared to urban (Table 1). Food was found to be the biggest area of expenditure in both rural and urban households, the food basket accounted for up to 36% of total income. Conclusions and significance: The cost of the food basket depends on household composition. Food costs rise as children grow older and this has potential health significance. Meat fruit and vegetables took up the largest share of the costs. Households on state benefits spend a larger percentage of take home income on food than households with an employed adult.
Keynote Forum
Theresa Loomis
University of Medicine and Dentistry of New Jersey USA
Keynote: Tackling Childhood Obesity and it’s Long Term Health Outcomes One Bite at a Time
Time : 10:10-10:45

Biography:
Dr. Loomis received her B.S from the University of Rhode Island and her M.S. and Doctorate of Clinical Nutrition from the University of Medicine and Dentistry of New Jersey. She is a Registered Dietitian (RD) with 16 years of experience in pediatric nutrition. Dr. Loomis has conducted presentations on a local and national level on a number of areas including the impact of Registered Dietitians in the Neonatal Intensive Care Unit (NICU), Combating Childhood obesity and Pediatric Food Allergies and Treating Picky Eating. Her doctoral work looked at the impact of standardized feeding guidelines for low birth weight infants, which was recently published in the Journal of Pediatric Gastroenterology and Nutrition. Dr. Loomis’ current research looks at the impact of nutrition counseling on childhood obesity, and the eating habits of picky eaters as well as the impact of role modeling on the eating habits and weight status of college students. Dr. Loomis is an Assistant Professor at SUNY Oneonta and is the Director of the Masters Program and Dietetics Internship. She also works as a pediatric dietitian in a pediatrician’s office counseling children who struggle with obesity and has owned her own private practice since 2010.
Abstract:
Childhood obesity is a growing concern worldwide. It has becoming a problem in every country where there is data. Children who are born preterm or Small for Gestational Age (SGA) are at higher risk for developing childhood obesity than their peers who are born on time and of normal weight. This presentation will discuss the impact that the development of obesity has not only on the more commonly known long term health consequences such as diabetes, hypertension and cardiovascular disease, but it will also discuss it’s impact on the development of food allergies and other inflammatory diseases. The eating habits during the perinatal period and breastfeeding and their impact on the development of obesity will also be described. We will explore the impact individual nutrition counseling has on childhood obesity compared to group counseling and virtual counseling. Finally evidenced based strategies to prevent the onset of obesity during pregnancy, breastfeeding and childhood will be presented.
Keynote Forum
Fatemeh Rabiee
Birmingham City University ,UK
Keynote: Community Based Childhood Obesity Intervention Programme: working with parents & schools in Birmingham, UK: challenges & opportunities
Time : 09:35-10:10

Biography:
Prof Fatemeh Rabiee is a professor in Public Health Promotion and a registered Public Health Nutritionist. She has extensive experience of teaching, research supervision, community based Public Health Nutrition Intervention Programme, capacity building and mentorship in Higher Education & Research in the UK, Netherlands, Uzbekistan & other countries of economic transition. Fatemeh has initiated, designed, managed and implemented a number of research and educational programme in the broad area of health and social policy; health inequalities, mental health promotion, public health nutrition and evaluation of health & social care projects nationally and internationally.
Her other specialist skills includes: Public Health Practitioner; working a day per week in practice in advisory capacity with a number of voluntary and statutory organizations, Advocacy, lobbying and campaigning; stakeholder engagement and deliberation, Public Health; policy, practice. Design, implement, and dissemination of science into policy and practice, Promoting health through community development and public engagement.
Abstract:
Statement of the Problem: Obesity is a key public health issue affecting both children and adults in developed countries and countries of economic transition (WHO, 2011). Childhood obesity pattern in UK is no different; a quarter of 2-10 and one third of 11-15 year old are overweight or obese (Public Health England, 2014). Obesity harms children’s health both physically and psychologically. Obesity is the outcome of a complex set of factors, its prevention and management therefore requires multiple set of action and life course approach ( Wyatt et al., 2013; Marmot, 2015). This paper begins with highlighting some of the main issues contributing to childhood obesity in the UK and moves on to argue the case for multifaceted investment in prevention.
Methodology & Theoretical Orientation: Using 3 cases studies from Children Centres, and Schools in the West Midlands, it compares the process of designing, recruiting participants and implementing “FABTots”, “MEND”, and “Make it Count” community based childhood obesity prevention programmes in diverse communities.
Findings and Discussion: Data highlights the impact and outcome of those 3 projects in childhood obesity and their influences on family dietary practices and food knowledge. It emphasis opportunities as well as constrains of working in community settings. It argues the importance of community development approach & the role of community engagement in goal setting and ownership of intervention programmes.
Recommendations: It concludes that although in most cases these intervention programmes were successful in developing skills and confidence in the respective communities, for sustainability of these programmes the complex impact of lifestyles choices and structural issues should not be overlooked.
- Bariatric surgery for obesity and metabolic disorder | Obesity
Location: 1
Session Introduction
Marek Benes
Institute of Clinical and Experimental Medicine, Czech Republic
Title: Final Results of Multi-Center, Prospective, Controlled Trial of the Duodeno-Jejunal Bypass Liner for the Treatment of Type 2 Diabetes Mellitus in Obese Patients: Efficacy and Factors Predicting a Suboptimal Effect
Time : 15:40-16:05

Biography:
Marek Benes M.D., born 1976 in Prague, where also graduated on 3rd Medical Faculty of Charles University in 2001, in this year started as physician on department of gastroenterology and hepatology in Institute of clinical and experimental medicine in Prague. Main subjects of interest are endoscopy and specially bariatric endoscopy. In present time we have biggest group of patients treated with gastro-jejunal bypass sleeve - Endobarrier in Europe.
Abstract:
Introduction: The global increase in obesity incidence results in an increase of type-2 diabetes mellitus (T2DM). Surgical treatment has proven to be effective; however it carries a high risk of complications. The duodenaljejunal bypass liner (EndoBarrier®, GI Dynamics and EB) is an endoscopic implant that mimics the intestinal bypass portion of the Roux-en-Y gastric bypass. It results in weight loss and improvements in glucose control in obese patients with T2 diabetes mellitus (T2DM).
Aims & Methods: This is a final report of a prospective, controlled, multi-centre study aimed to determine the effectiveness of EB and to identify factors associated with a sub-optimal outcome of EB.
Results: Seventy (70) subjects (45 with an implant, 25 controls) were included in the study. The groups were comparable with respect to age, gender, BMI (mean 41.7 vs. 39.5 kg/m2), T2DM duration (7.8 vs. 8.3 years), HbA1c level (88 vs. 86 mmol/mol) and T2DM treatment. In the EB group, all devices were successfully implanted. Only 6 devices had to be explanted prior to the end of the 10 months study period (bleeding, dislocation and need for ERCP because of choledocholithiasis). The mean procedure time was 17 minutes for an implantation and 16 minutes for an explanation. At 10 months there was significantly greater weight loss and %EWL (19% vs. 7% and 43 vs. 12) and significantly improved long-term compensation of T2DM marker HbA1c (decreased by 25 vs. 10 mmol/mol) in the EB group. T2DM medicinal treatment could be reduced in more device subjects than controls. There was no serious adverse event. Mild abdominal pain and nausea after implantation were experienced by 60% of patients during first 14 days after implantation, 30% of patients during the first month and 10% of patients after one month. Lower initial BMI and lower body height were identified as negative prognostic factors for pain, but positive for efficacy of EB.
Conclusion: The EB is safe when implanted for 10 months and results in significant weight loss and HbA1c reduction. This suggests that this novel device is a candidate for the primary therapy of morbid obesity and T2DM. Lower initial BMI and lower body height could be negative prognostic factor for pain, but positive for efficacy.
Reshma Ramracheya
University of Oxford, UK
Title: Unravelling the role of the gut hormone PYY in diabetes remission and pancreatic islet function following Roux-En-Y gastric bypass
Time : 16:30-16:55

Biography:
Dr. Reshma Ramracheya investigate the regulation and failure of the insulin-secreting beta-cell and glucagon-secreting alpha-cell in normal health and diabetes respectively. As an islet physiologist, She intrigued by how pancreatic islet cells, despite being biochemically similar, are able to respond to nutrients and drugs differently. Type 2 diabetes is a global epidemic with over 300 million sufferers worldwide. It results from a combination of insufficient insulin secretion and over-secretion of glucagon but the role of glucagon as a counter-regulatory hormone in diabetes has been largely overlooked.Her group is investigating the effects of weight-loss surgery and the appetite-regulating hormone peptide tyrosine tyrosine (PYY) on pancreatic islet secretion and in human diabetes. In parallel, they are also studying the mechanism by which the gut hormone glucagon-like peptide 1 (GLP-1) inhibits glucagon secretion in human isolated islets.
Abstract:
Roux-En-Y gastric bypass (RYGB) results in long-lasting remission from type-2 diabetes (T2D) in most cases. Improvements in glucose homeostasis occur within days of surgery, but the mechanisms involved remain unclear. Although pancreatic islets play a fundamental role in glucose homeostasis, the impact of RYGB on islet architecture and secretory properties has not been studied thoroughly. T2D is a bihormonal disease characterised by both insufficient insulin secretion and impairment in glucagon regulation. Whether RYGB can correct both hormonal secretory defects remain unexplored.
Using the Goto-Kakizaki (GK) rat model of T2D, we have explored whether RYGB affects islet structure and glucose-stimulated insulin secretion (GSIS) and glucagon release. RYGB restored ‘distorted’ islets from diabetic rats to spheroidal shape as in healthy animals. Compared to the sham-operated animals, RYGB normalised glucose-dependent glucagon and insulin secretion. Thus, islets from RYGB rats exhibited markedly enhanced insulin secretion at 20mM glucose and complete restoration of glucose-induced suppression of glucagon release.
Culture of isolated islets with serum from RYGB animals resulted in improved insulin and glucagon secretion, in support of a humoral factor which remains conserved in serum. These effects were reversed following immuno-neutralization of the gut hormone peptide tyrosine tyrosine (PYY) but persisted in the presence of a glucagon-like peptide-1 (GLP-1) receptor antagonist. Chronic (60-72h) treatment of islets with synthetic PYY enhanced GSIS in a NPY1-receptor-dependent manner. PYY application also restored GSIS and normalised impaired glucose-induced glucagon release in islets from severely diabetic GK rats and human donors with T2D. These data provide a novel mechanistic insight on the effect of RYGB in diabetes and highlight that the mechanism behind the improvement of islet function is dependent on PYY, and not GLP-1.
These findings imply that a pharmacological agent enhancing PYY release or its action could provide an effective and non-surgical therapy for T2D.
Sukaina Jaffar
Department of Surgery, Nepean Hospital
Title: Multi-dimensional validated reporting of dysphagia post sleeve gastrectomy

Biography:
Abstract:
Background: Few studies have reported the prevalence of dysphagia, as its own clinical entity in the bariatric population; without being examined under the umbrella of gastro-oesophageal reflux disease. This is compounded by studies not outlining methodologies used to assess dysphagia. Moreover, varying follow-up periods and different bariatric procedures have led to conflicting results.
Objectives: To assess the prevalence of dysphagia using a statistically robust patient-reported tool, Dysphagia Handicap Index (DHI) post Laparoscopic Sleeve Gastrectomy (LSG). DHI is a validated tool which additionally measures the handicapping effects of dysphagia on emotional and functional domains of living. Methods: DHI questionnaire was administered to 124 patients who underwent LSG at least 1 year prior. Post-operative weight, change in BMI, percent Total Weight Loss (%TWL) and percent Excess Weight Loss (%EWL) were calculated. Physical, emotional and functional subscales were analyzed separately and altogether. Three additional questions were added to the DHI to delineate oesophageal dysphagia.
Results: Average pre-operative weight and BMI is 123.8 kg and 43 kg/m2, respectively. Median %TWL and %EWL are 32% and 76.2%, respectively. An average reduction in BMI value of 14 kg/m2 was found. 41% of our cohort reported to mild dysphagia and 54% reported moderate to severe dysphagia based on the Modified DHI Score (DHI+Oesophageal Specific Dysphagia Score). No patient required corrective intervention. Patients reporting higher DHI scores were less likely to achieve the median TWL of 35.4 kg (OR 0.40, 95% CI 0.17-0.91). Dysphagia is a common symptom reported in our cohort and was found to have an impact on weight loss outcomes.
Conclusion: Prospective, single-institution analysis using a validated tool reveals post-operative dysphagia to be a common clinical entity in our population with functional and psychological influences.
Biography:
Attila Seyhan was an Assoc. Prof. at the Translational Research Institute for Metabolism and Diabetes, Florida Hospital, an Adjunct Prof. at Sanford-Burnham Prebys Medical Discovery Institute, Orlando, FL and a Research Affiliate with the Department of Chemical Engineering, MIT.
Previously he was in pharmaceutical (Pfizer, Wyeth) and biotech (OpenBiosystems, Dharmacon, Somagenics) in leading positions. He has 16+ years of experience in drug/target/ biomarker discovery and development, preclinical/clinical Translational Research in metabolic diseases/diabetes, cancer, inflammation & immunology, and viral pathogens (HCV, HIV, Semliki forest virus) in leading positions. He has published 35+ scientific articles and book chapters and is an inventor/co-inventor of more than 9 issued US patents and several pending applications. He has successfully authored/co-authored over 14 grant proposals totaling $6.2 million, including a Biodefense grant from the US Department of Defense, NIH and Pharma. He has earned several awards including a doctoral fellowship from NATO, Pfizer Excellence Award for contributions towards Biomarkers of Lupus Disease Study
Abstract:
- Young Researchers Forum
Session Introduction
Maryam Pishsaraeian
Meshkat School, Iran
Title: The evolution of aerobic activity on the level of IgA immunoglobulin in female teenager students
Time : 16:45-17:10

Biography:
M Pishsaraeian has completed her MS degree in Exercise Physiology from University of Mazandaran, Babolsar. Iran. She is a teacher of Sport Science in High School of Tehran city and her field of interest is the evaluation of effects of sport and exercise on psychological and physiological factors.
Abstract:
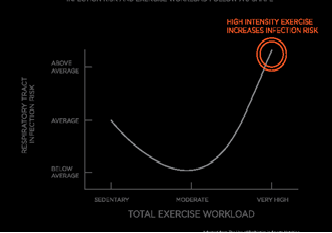
Obesity is a major problem in many societies. One of the proposed solutions for the treatment of obesity is exercise. Exercise has complex effects on immune system. One of most important immunoglobulins in mucus is IgA that protect the body against microorganisms. The aim of this study was to evaluate the effect of aerobic exercise on the levels of IgA and total protein in salivary of female teenager students. 20 female healthy volunteer students (age 12-13) without any infection, using drug, cardiovascular diseases and with healthy diet randomly divided into control (n=10) and aerobic activity (n=10) groups. Before the exercise saliva samples were taken from each student and kept in suitable condition. Aerobic activity group performs the Shuttle Run Test for exercise and control group has no activity. After finishing the exercise the samples were collected and sent to laboratory for analysis. For detection of IgA the ELISA kit essay was used and the Bradford protein essay was used for the detection of total protein. Our results have indicated that in comparison with pre-test and post-test of aerobic activity group, the level of IgA concentration was significantly (P≤0/05) decreased but the total protein was increased (P≤0/05) significantly. There has been no significant change in the level of IgA between two groups. It is recommended that duration, type and intensity of physical activity be considered for prevention of infection.
- Obesity
Session Introduction
Sandra Jumbe
Doctor
Title: Post-surgical cliff after bariatric surgery: accounts of patients and their health care professionals

Biography:
Sandra is a health psychologist with research interests in chronic disease management and smoking cessation. She recently completed her doctorate in health psychology at the University of the West of England in Bristol, UK. She previously worked in the National Health Service (NHS) as a primary care and mental health researcher, an assistant psychologist and in research governance. She has also delivered consultancy work developing tailored stress management interventions within organisations and group settings. Alongside her research work, Sandra also works as a general advisor for the London Research Design Service team based at Queen Mary University, which involves supporting health professionals and research teams within the North East London area to develop their research ideas into full funding applications to the NIHR and other peer reviewed funders
Abstract:
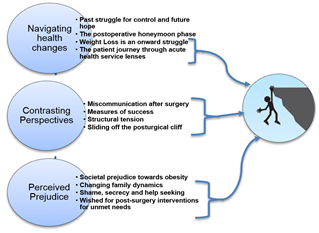
Statement of the problem: The superiority of bariatric surgery for improving medical outcomes in severely obese individuals when compared to other weight loss interventions remains undisputed. However, knowledge about the psychological impact of the procedure on people’s lives is limited. Recent systematic reviews have shown persisting disordered psychosocial wellbeing after surgery when compared to control groups, especially after long-term monitoring, suggesting need for psychological support and longer term postoperative research on psychological outcomes. Research literature infers limited understanding regarding the postoperative lived experience from the patient perspective. This may form a barrier in health professionals’ understanding of this patient group’s postoperative ongoing needs. This study aimed to capture patients and health professionals’ accounts of the postoperative bariatric surgery experience, exploring concordance between the two groups to gauge awareness of patients’ subsequent health needs
- Bariatric surgery for obesity and metabolic disorder
Location: Olimpica 4
Session Introduction
Sukaina Jaffar
Nepean Hospital, Australia
Title: Correlation between Laparoscopic Sleeve Gastrectomy outcomes and Mental Health
Time : 15:50-16:15

Biography:
Abstract:
Sukaina Jaffar
Nepean Hospital, Australia
Title: Correlation between Laparoscopic Sleeve Gastrectomy outcomes and Mental Health

Biography:
Abstract:
- Obesity
Location: Olimpica 4
Session Introduction
Dr. Sandra Jumbe
Queen Mary University of London, UK
Title: Post-surgical cliff after bariatric surgery: accounts of patients and their health care professionals

Biography:
Sandra is a health psychologist with research interests in chronic disease management and smoking cessation. She recently completed her doctorate in health psychology at the University of the West of England in Bristol, UK. She previously worked in the National Health Service (NHS) as a primary care and mental health researcher, an assistant psychologist and in research governance. She has also delivered consultancy work developing tailored stress management interventions within organisations and group settings. Alongside her research work, Sandra also works as a general advisor for the London Research Design Service team based at Queen Mary University, which involves supporting health professionals and research teams within the North East London area to develop their research ideas into full funding applications to the NIHR and other peer reviewed funders
Abstract:
- Types of bariatric surgery
Location: Olimpica 4
Session Introduction
Matteo Catanzano
Department of Surgery, Aberdeen Royal Infirmary, Aberdeen, UK
Title: Stapless laparoscopic sleeve gastrectomy: reasoning and technical insights
Biography:
Dr. Matteo Catanzano has completed his MBChB, at the University of Glasgow, where he started carrying out research, something he has continued now that he is in his second year of foundation training, as a part of the Bariatric Surgery team in the Aberdeen Royal Infirmary.
Abstract:
Introduction: Laparoscopic sleeve gastrectomy (LSG) with staple line reinforcement (SLR) is a popular and safe treatment option for morbid obesity, yet its benefits remain inaccessible to many, especially in developing countries, due to the high cost of the equipment required.
Objective: Devise and describe a modified, stapless laparoscopic sleeve gastrectomy that is as safe as standard LSG with SLR, but costs less.
Methods: Analysis of the influence of technical adaptations on the outcome of LSG was performed in a case–series of 3 patients. The main modification adapted was performing the closure of the stomach stapless. The primary outcome was the occurrence of leak post-op. The secondary outcomes were: operative time, prolonged hospital stay, % excess weight loss at 6 months and 12 months.
Results: Median operative time and hospital stay were 132 min and 2 days. No post-op leaks were recorded. The median excess weight loss at 6 months was 39% and at 1 year 57.7%.
Conclusion: Stapless LSG is an affordable alternative to the standard LSG techniques, both in terms of financial costs and complications rate
- Gastric Bypass Surgery
Location: Olimpica 4
Session Introduction
Mohos Elemer
Veszprem County Hospital, Hungary
Title: Single centre results after 588 laparoscopic Roux –en-Y gastric bypass and 57 laparoscopic gastric sleeve resections performed in Hungary between 2010 and 2017
Biography:
Mohos Elemer is currently working Veszprem County Hospital, Hungary. He published many articles about his field of Bariatric Surgery in different Journals.
Abstract:
Dr. Aly Elbahrawy
Surgeon, McGill University Health Center Montreal General Hospital.
Title: Laparoscopic wedge resection of gastrojejunostomy for weight recidivism after gastric bypass
Biography:
Dr. Ely Elbahrawy is working in Department of Surgery, and Division of General Surgery, Center for Bariatric Surgery, McGill University Health Center Montreal General Hospital, 1650 Cedar Avenue, Canada.
Abstract:
Background & Aim: Weight recidivism after Roux-en-Y gastric bypass (RYGB) is a common problem. Often, this weight loss failure or regain may be due to a wide gastrojejunostomy (GJ). We evaluated the feasibility and safety of a novel approach of laparoscopic wedge resection of gastrojejunostomy (LWGJ) for a wide stoma after RYGB associated with weight recidivism.
Methods: This is a single-center retrospective study of a prospectively-collected database. We analyzed outcomes of patients with weight recidivism after RYGB and a documented wide GJ (>2 cm) on imaging, who underwent LWGJ between 11/2013-05/2016.
Results: Nine patients underwent LWGJ for dilated stomas. All patients were female with a mean±SD age of 53±7 years. Mean interval between RYGB and LWGJ was 9±3 years. All cases were performed laparoscopically with no conversions. Mean operative time and hospital stay were 86±9 minutes and 1.2±0.4 days, respectively. The median (IQR) follow-up time was 14 (12-18) months. During follow-up, there were no deaths, postoperative complications or unplanned readmissions or reoperations. The mean and median (IQR) BMI before RYGB and LWGJ were 55.4±8.1 kg/m2 and 56.1 (47.9-61.7) and 43.4±8.6 kg/m2 and 42.1 (38.3-47.1), respectively. One year after LWGJ, mean and median (IQR) BMI significantly decreased to 34.9±7.3 kg/m2 and 33.3 (31.7-35.0) corresponding to a mean %EWL of 64.6±19.9 (P<0.05).
Conclusion: LWGJ is safe and can lead to further weight loss in patients experiencing weight recidivism after RYGB with a wide GJ (>2 cm). Long-term follow-up is needed to determine the efficacy and durability of LWGJ and compare its outcomes with other endoscopic/surgical approaches for weight recidivism after RYGB with a documented wide GJ.
