Day 2 :
Keynote Forum
Claudio Blasi
ASLRMB-1D hospital diabetes center, Italy
Keynote: The vagal system as a mediator of the therapeutic effects of bariatric surgery
Time : 10:35-11:10

Biography:
Dr. Claudio Blasi graduated in medicine from Rome “La Sapienza” University at the age of 27 and did a postgraduate specialization in endocrinology at “La Sapienza” School of Medicine. He has been the director of the ASLRMB-1D hospital diabetes center in Rome. He has published more than 30 papers in reputed journals.
Abstract:
Obesity and type 2 diabetes are chronic diseases that respond with difficulty to drug therapies and lifestyle changes. At the origin of this resistance to treatment, an alteration in the functioning of brain sectors in charge of the reward system and of the energy homeostasis, due to a modification of synaptic transmission, has been hypothesized. Overfeeding, presumably beginning as a psychological compulsive search for a rewarding stimulus, turns into food addiction due to the adaptation of synapses in the reward circuit in response to the increased intensity of the inputs (synaptic plasticity). The same would apply to the brain areas responsible for the maintenance of energy homeostasis. The afferent vagal paths transmit to the brain information about ingested food from the digestive tract. Their intermediate station in the brainstem, the vagal nucleus of the solitary tract, has an important role in modulating the metabolic function of the liver and the pancreas. Moreover, they work as a channel for the transmission of information from the periphery to the CNS with regard to both favorable and adverse events. In this way, they influence the synaptic activity of various brain areas through neuroplasticity. The profound anatomical and functional changes in the vagal system caused by bariatric surgery could explain the dramatic improvement in diabetes and the renewed sensitivity to diet by a normalization of synaptic activity. In the future, modulating pharmacologically vagus-vagal synaptic connections or driving brain plasticity via stimulation of the vagus afferents could obtain, “knifelessly”, the same therapeutic effects as surgery.
Keynote Forum
Signe Sørensen Torekov
University of Copenhagen, Denmark
Keynote: Obesity and GLP-1. Obesity pathophysiology and GLP-1 treatment potential
Time : 11:10-11:45

Biography:
Associate Professor Signe Torekov has a strong background in metabolic translational research.
In collaboration with University of California her research has shown that infusion of the natural appetite hormone GLP-1 inhibits appetite and lowers blood glucose (2 first authorships in Diabetes, Obesity and Metabolism (Impact factor (IF) 6.2), 2011 and 2013). During the last three years, her research team has discovered that: 1) obese people have low endogenous GLP-1 response (first author in Diabetes (IF8.4), 2015); 2) weight loss induces a marked increase in GLP-1 response and that this is part of a successful maintenance of weight loss (last author in European Journal of endocrinology (IF4.1), 2016) (major media exposure: front page interview of The Times and live on BBC Today, April 2016 (7 mill listeners), and 3) treatment with GLP-1 analogues facilitate long term weight loss maintenance accompanied by substantial improvement in metabolic health, compared to diet-induced weight loss maintenance (Last author in Journal of Clinical Endocrinology and Metabolism (IF6.4) and International Journal of Obesity (IF5.4), 2015). Furthermore, by synergistically integrating metabolic physiology with novel state of the art mass spectrometry based proteomics and metabolomics, in collaboration with Professor Matthias Mann, Max Planck Institute, they have designed a novel experimental approach for clinical translational metabolism in order to identify new health markers in obesity (2. last author in Molecular Systems Biology, (IF 12.3) and last author in Metabolomics (IF3.7), 2016). In addition, Signe Torekov was awarded Major Discovery 2010-2015 for the her first author paper in Diabetes (IF8.4) 2014 where she, together with the research team, showed that Long QT Syndrome patients with mutations in KCNQ1 besides having prolonged cardiac arrhythmia, also have hyperinsulinemic hypoglycemia. More recently, Signe Torekov has shown that Long QT Syndrome patients with loss of function mutations in hERG display exaggerated incretin and endocrine pancreatic function and thus increased risk of symptomatic reactive hypoglycemia. Pharmacological blockade in rats and inhibition of hERG in β and L- cells had similar effects. Hypoglycemia leads to increased propensity for arrhythmias; hypoglycemia may therefore even further increase the risk of malignant arrhythmia in LQTS patients (published in Circulation (IF17) with Dr. Torekov as last and corresponding author).
Abstract:
Obesity impairs almost all aspects of health and is a global challenge to our healthcare system as the prevalence reaches 1 billion humans. Therefore, there is an acute need for better prevention and treatment strategies. Glucagon-like-peptide-1 (GLP-1), secreted from endocrine cells in the intestine upon meal intake, reduces food intake. We have previously shown that: 1) obese people have low endogenous GLP-1 response; 2) weight loss induces a marked increase in GLP-1 response, and 3) treatment with GLP-1 analogues facilitates long term weight loss maintenance (12 kg) accompanied by substantial improvement in metabolic health, compared to diet-induced weight loss maintenance. Chronic inflammation is an established part of the pathogenesis of obesity, and activation of macrophages and T cells in the expanded adipose tissue is coupled to the development of a pro-inflammatory state and insulin resistance. Interestingly, emerging evidence identifies GLP-1 as a potentially important immuno-modulator. GLP-1 decreases inflammation-associated gene and protein expression in macrophages and exerts anti-inflammatory actions in adipocytes and endothelial cells as well as potent anti-inflammatory effects in humans.
Keynote Forum
Signe Torekov
Associate Professor
Keynote: Obesity and GLP-1. Obesity pathophysiology and GLP-1 treatment potential
Time : 11:10-11:45

Biography:
Associate Professor Signe Torekov has a strong background in metabolic translational research.
In collaboration with University of California her research has shown that infusion of the natural appetite hormone GLP-1 inhibits appetite and lowers blood glucose (2 first authorships in Diabetes, Obesity and Metabolism (Impact factor (IF) 6.2), 2011 and 2013). During the last three years, her research team has discovered that: 1) obese people have low endogenous GLP-1 response (first author in Diabetes (IF8.4), 2015); 2) weight loss induces a marked increase in GLP-1 response and that this is part of a successful maintenance of weight loss (last author in European Journal of endocrinology (IF4.1), 2016) (major media exposure: front page interview of The Times and live on BBC Today, April 2016 (7 mill listeners), and 3) treatment with GLP-1 analogues facilitate long term weight loss maintenance accompanied by substantial improvement in metabolic health, compared to diet-induced weight loss maintenance (Last author in Journal of Clinical Endocrinology and Metabolism (IF6.4) and International Journal of Obesity (IF5.4), 2015). Furthermore, by synergistically integrating metabolic physiology with novel state of the art mass spectrometry based proteomics and metabolomics, in collaboration with Professor Matthias Mann, Max Planck Institute, they have designed a novel experimental approach for clinical translational metabolism in order to identify new health markers in obesity (2. last author in Molecular Systems Biology, (IF 12.3) and last author in Metabolomics (IF3.7), 2016). In addition, Signe Torekov was awarded Major Discovery 2010-2015 for the her first author paper in Diabetes (IF8.4) 2014 where she, together with the research team, showed that Long QT Syndrome patients with mutations in KCNQ1 besides having prolonged cardiac arrhythmia, also have hyperinsulinemic hypoglycemia. More recently, Signe Torekov has shown that Long QT Syndrome patients with loss of function mutations in hERG display exaggerated incretin and endocrine pancreatic function and thus increased risk of symptomatic reactive hypoglycemia. Pharmacological blockade in rats and inhibition of hERG in β and L- cells had similar effects. Hypoglycemia leads to increased propensity for arrhythmias; hypoglycemia may therefore even further increase the risk of malignant arrhythmia in LQTS patients (published in Circulation (IF17) with Dr. Torekov as last and corresponding author).
Abstract:
Obesity impairs almost all aspects of health and is a global challenge to our healthcare system as the prevalence reaches 1 billion humans. Therefore, there is an acute need for better prevention and treatment strategies. Glucagon-like-peptide-1 (GLP-1), secreted from endocrine cells in the intestine upon meal intake, reduces food intake. We have previously shown that: 1) obese people have low endogenous GLP-1 response; 2) weight loss induces a marked increase in GLP-1 response, and 3) treatment with GLP-1 analogues facilitates long term weight loss maintenance (12 kg) accompanied by substantial improvement in metabolic health, compared to diet-induced weight loss maintenance. Chronic inflammation is an established part of the pathogenesis of obesity, and activation of macrophages and T cells in the expanded adipose tissue is coupled to the development of a pro-inflammatory state and insulin resistance. Interestingly, emerging evidence identifies GLP-1 as a potentially important immuno-modulator. GLP-1 decreases inflammation-associated gene and protein expression in macrophages and exerts anti-inflammatory actions in adipocytes and endothelial cells as well as potent anti-inflammatory effects in humans.
Keynote Forum
Signe Torekov
Associate Professor
Keynote: Obesity and GLP-1. Obesity pathophysiology and GLP-1 treatment potential
Time : 11:10-11:45

Biography:
Associate Professor Signe Torekov has a strong background in metabolic translational research.
In collaboration with University of California her research has shown that infusion of the natural appetite hormone GLP-1 inhibits appetite and lowers blood glucose (2 first authorships in Diabetes, Obesity and Metabolism (Impact factor (IF) 6.2), 2011 and 2013). During the last three years, her research team has discovered that: 1) obese people have low endogenous GLP-1 response (first author in Diabetes (IF8.4), 2015); 2) weight loss induces a marked increase in GLP-1 response and that this is part of a successful maintenance of weight loss (last author in European Journal of endocrinology (IF4.1), 2016) (major media exposure: front page interview of The Times and live on BBC Today, April 2016 (7 mill listeners), and 3) treatment with GLP-1 analogues facilitate long term weight loss maintenance accompanied by substantial improvement in metabolic health, compared to diet-induced weight loss maintenance (Last author in Journal of Clinical Endocrinology and Metabolism (IF6.4) and International Journal of Obesity (IF5.4), 2015). Furthermore, by synergistically integrating metabolic physiology with novel state of the art mass spectrometry based proteomics and metabolomics, in collaboration with Professor Matthias Mann, Max Planck Institute, they have designed a novel experimental approach for clinical translational metabolism in order to identify new health markers in obesity (2. last author in Molecular Systems Biology, (IF 12.3) and last author in Metabolomics (IF3.7), 2016). In addition, Signe Torekov was awarded Major Discovery 2010-2015 for the her first author paper in Diabetes (IF8.4) 2014 where she, together with the research team, showed that Long QT Syndrome patients with mutations in KCNQ1 besides having prolonged cardiac arrhythmia, also have hyperinsulinemic hypoglycemia. More recently, Signe Torekov has shown that Long QT Syndrome patients with loss of function mutations in hERG display exaggerated incretin and endocrine pancreatic function and thus increased risk of symptomatic reactive hypoglycemia. Pharmacological blockade in rats and inhibition of hERG in β and L- cells had similar effects. Hypoglycemia leads to increased propensity for arrhythmias; hypoglycemia may therefore even further increase the risk of malignant arrhythmia in LQTS patients (published in Circulation (IF17) with Dr. Torekov as last and corresponding author).
Abstract:
Obesity impairs almost all aspects of health and is a global challenge to our healthcare system as the prevalence reaches 1 billion humans. Therefore, there is an acute need for better prevention and treatment strategies. Glucagon-like-peptide-1 (GLP-1), secreted from endocrine cells in the intestine upon meal intake, reduces food intake. We have previously shown that: 1) obese people have low endogenous GLP-1 response; 2) weight loss induces a marked increase in GLP-1 response, and 3) treatment with GLP-1 analogues facilitates long term weight loss maintenance (12 kg) accompanied by substantial improvement in metabolic health, compared to diet-induced weight loss maintenance. Chronic inflammation is an established part of the pathogenesis of obesity, and activation of macrophages and T cells in the expanded adipose tissue is coupled to the development of a pro-inflammatory state and insulin resistance. Interestingly, emerging evidence identifies GLP-1 as a potentially important immuno-modulator. GLP-1 decreases inflammation-associated gene and protein expression in macrophages and exerts anti-inflammatory actions in adipocytes and endothelial cells as well as potent anti-inflammatory effects in humans.
Keynote Forum
Lenwood W. Hayman
University of Michigan, USA
Keynote: Keynote: Development and Validation of the Children’s Emotional Eating Scale (ChEES)
Time : 09:05-09:40

Biography:
Lenwood Hayman, Assistant Professor of Public Health at the University of Michigan – Flint, focuses on the psychosocial determinants of eating behaviors in under-privileged communities. Specifically, Lenwood’s research focuses on the assessment of emotional eating (including stressed and bored eating) in preschool-aged children from low-income families. Lenwood has also worked with community-based organizations to demonstrate how increased participation in local food systems correlates with eating a healthier diet. Recently, Lenwood established the Mindful Promotion of Healthy Eating & Learning (Mind-PHEL) research team in which he studies the influence of mindfulness-based activities on healthy eating and positive student learning outcomes. Lenwood is in the process of developing a mindfulness-based intervention to encourage healthy eating behaviors in low-income communities.
Abstract:
Associations between the propensity to eat foods high in sugar and fat in response to negative emotions has been linked to a higher risk of obesity in multiple prior studies in adults. Emotional eating, however, has not been extensively studied in children, particularly among very young children from low-income families. Research suggests that low-income mothers of preschool-aged children believe that children in this age range can eat in response to their emotions, however, they tend to underreport the occurrence of emotional eating for their own children. Such findings could be due, in part, to the fact that the two most commonly-used questionnaires were developed in White, European populations. Due to contradicting evidence regarding the utility of current questionnaires to reliably assess emotional eating in very young children from low-income families in the United States, the focus of the current study was to develop such a scale. Specifically, we used a 2-aim, mixed-methods, cross-sectional design to develop a valid tool for assessing emotional eating at a population level in very young children from low-income families. In our previous work, we qualitatively assessed how mothers from US-based low-income populations conceptualized the construct of emotional-eating in preschool-aged children. We then used that data to develop an inventory of items to capture the salient aspects of emotional eating. These items were assessed by a sample of mothers from the target population for clarity and relatability. Those items demonstrating face- and content-validity, along with the child version of the Dutch Eating Behavior Questionnaire, were then used to collect data from a sample of 200 participants from the target population. Results and conclusions will be discussed in detail during conference session.
- Young Researchers Forum
Session Introduction
Maryam Pishsaraeian
Meshkat School, Iran
Title: The evolution of aerobic activity on the level of IgA immunoglobulin in female teenager students
Time : 16:45-17:10

Biography:
M Pishsaraeian has completed her MS degree in Exercise Physiology from University of Mazandaran, Babolsar. Iran. She is a teacher of Sport Science in High School of Tehran city and her field of interest is the evaluation of effects of sport and exercise on psychological and physiological factors.
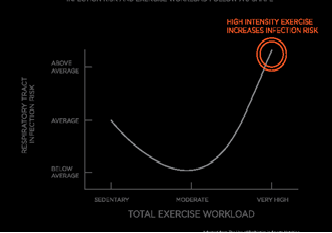
Abstract:
Obesity is a major problem in many societies. One of the proposed solutions for the treatment of obesity is exercise. Exercise has complex effects on immune system. One of most important immunoglobulins in mucus is IgA that protect the body against microorganisms. The aim of this study was to evaluate the effect of aerobic exercise on the levels of IgA and total protein in salivary of female teenager students. 20 female healthy volunteer students (age 12-13) without any infection, using drug, cardiovascular diseases and with healthy diet randomly divided into control (n=10) and aerobic activity (n=10) groups. Before the exercise saliva samples were taken from each student and kept in suitable condition. Aerobic activity group performs the Shuttle Run Test for exercise and control group has no activity. After finishing the exercise the samples were collected and sent to laboratory for analysis. For detection of IgA the ELISA kit essay was used and the Bradford protein essay was used for the detection of total protein. Our results have indicated that in comparison with pre-test and post-test of aerobic activity group, the level of IgA concentration was significantly (P≤0/05) decreased but the total protein was increased (P≤0/05) significantly. There has been no significant change in the level of IgA between two groups. It is recommended that duration, type and intensity of physical activity be considered for prevention of infection.
- Bariatric surgery for obesity and metabolic disorder
Location: Olimpica 4
Session Introduction
Sukaina Jaffar
Nepean Hospital, Australia
Title: Correlation between Laparoscopic Sleeve Gastrectomy outcomes and Mental Health
Time : 15:50-16:15

Biography:
Abstract:
Sukaina Jaffar
Nepean Hospital, Australia
Title: Correlation between Laparoscopic Sleeve Gastrectomy outcomes and Mental Health

Biography:
Abstract:
- Obesity
Location: Olimpica 4
Session Introduction
Dr. Sandra Jumbe
Queen Mary University of London, UK
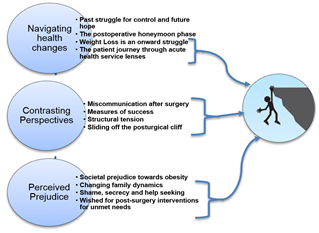
Title: Post-surgical cliff after bariatric surgery: accounts of patients and their health care professionals

Biography:
Sandra is a health psychologist with research interests in chronic disease management and smoking cessation. She recently completed her doctorate in health psychology at the University of the West of England in Bristol, UK. She previously worked in the National Health Service (NHS) as a primary care and mental health researcher, an assistant psychologist and in research governance. She has also delivered consultancy work developing tailored stress management interventions within organisations and group settings. Alongside her research work, Sandra also works as a general advisor for the London Research Design Service team based at Queen Mary University, which involves supporting health professionals and research teams within the North East London area to develop their research ideas into full funding applications to the NIHR and other peer reviewed funders
Abstract: